How Long Does Suboxone Block Opioids? Discover the Duration and Effects17 min read
Are you struggling with opioid addiction or know someone who is? Suboxone can be a game-changer in the journey to recovery. But have you ever wondered how long it actually blocks opioids and helps in the recovery process? In this comprehensive article, we’ll delve into the duration and effects of Suboxone, providing you with valuable insights to make informed decisions on your path to recovery.
- 1. Mechanism of Suboxone: Learn how Suboxone works in the body to block opioids and alleviate withdrawal symptoms.
- 2. Factors Affecting Duration: Understand the various factors that influence how long Suboxone remains effective in blocking opioids.
- 3. Short-Term Effects: Explore the immediate actions of Suboxone on opioid receptors and how it helps manage withdrawal symptoms and cravings.
- 4. Duration of Suboxone’s Blockade: Dive into the details of how Suboxone’s active ingredients interact with opioid receptors and the duration of their effects.
- 5. Different Suboxone Formulations: Compare sublingual tablets, sublingual films, and injectable formulations concerning their effectiveness and duration of action.
- 6. Managing Suboxone Treatment: Discover the importance of medical supervision and personalized treatment plans to ensure successful recovery with Suboxone.
How Does Suboxone Work in the Body?
Suboxone contains two main active ingredients: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, meaning it binds to opioid receptors but produces weaker effects compared to full agonists like heroin or oxyco This binding action helps prevent withdrawal symptoms and cravings without inducing the intense euphoria associated with opioids. Naloxone, on the other hand, is an opioid antagonist that blocks the effects of other opioids. The combination of these two ingredients makes Suboxone an effective tool in the treatment of opioid addiction.
Factors Affecting Suboxone’s Duration
The duration of Suboxone’s action can vary from person to person due to several factors. Dosage and administration play a crucial role; higher doses may extend the blockade, but they can also increase the risk of side effects. Individual variability, including genetic factors and metabolism, influences how the body processes and responds to Suboxone. Additionally, the liver’s ability to metabolize buprenorphine and naloxone and the rate of urinary excretion can impact the overall duration of Suboxone’s effects.
The Importance of Proper Dosage and Administration
- Sublingual Administration: Suboxone is typically taken as a sublingual tablet or film, placed under the tongue for absorption. This method allows for quicker onset and a more sustained effect.
- Injectable Formulations: Extended-release Suboxone injections are available for some patients, offering longer-lasting effects and reducing the need for frequent dosing.
Individual Variability and Its Impact
- Genetic Factors: Genetic variations can influence how enzymes in the liver metabolize Suboxone, affecting its duration and overall efficacy.
- Metabolism Rate: Differences in individual metabolism can result in varying rates of drug clearance, leading to differences in how long Suboxone stays active in the body.
Metabolism and Excretion
- Liver Processing: Buprenorphine and naloxone are primarily metabolized by the liver, and liver function can impact the duration of Suboxone’s effects.
- Urinary Excretion: After metabolism, the breakdown products of Suboxone are eliminated from the body through urine. Factors affecting urinary excretion can influence the duration of action.
Short-Term Effects of Suboxone
Suboxone’s short-term effects are primarily focused on providing relief from opioid withdrawal symptoms and reducing cravings. When taken as prescribed, it quickly binds to opioid receptors, alleviating physical discomfort and stabilizing neurochemical imbalances. This action helps individuals to function more normally, as it reduces the overwhelming urge to use opioids. However, Suboxone’s effects may vary depending on factors such as dosage, individual response, and the severity of opioid dependence.
Immediate Actions on Opioid Receptors
Suboxone’s buprenorphine component binds to opioid receptors with high affinity, effectively blocking other opioids from attaching to these receptors. This competitive binding mechanism helps reduce the euphoric effects of opioids and diminishes the risk of overdose. Additionally, Suboxone’s partial agonist action leads to a gradual onset of effects, preventing the intense “rush” associated with full opioid agonists.
Suppression of Withdrawal Symptoms
- Reduction of Physical Discomfort: Suboxone’s activation of opioid receptors helps to alleviate physical withdrawal symptoms, such as muscle pain, nausea, and sweating.
- Normalization of Neurotransmitter Activity: Opioid withdrawal disrupts the balance of neurotransmitters in the brain. Suboxone helps restore this balance, improving mood and reducing anxiety.
- Stabilization of Vital Signs: During withdrawal, blood pressure and heart rate may fluctuate. Suboxone’s calming effect on the central nervous system helps stabilize these vital signs.
Reduction of Opioid Cravings
Suboxone’s long-lasting effects on opioid receptors help manage cravings effectively. By occupying these receptors, Suboxone prevents opioids from binding and triggering intense cravings. The reduction of cravings enables individuals to focus on their recovery journey and engage more effectively in therapy and other supportive treatments.
Dopaminergic Pathways and Craving Management
- Impact on Reward Pathways: Opioids stimulate the release of dopamine, leading to intense feelings of pleasure. Suboxone’s partial activation of these pathways helps minimize cravings by providing some level of satisfaction without inducing euphoria.
- Psychological Effects on Cravings: The psychological aspect of addiction plays a crucial role in cravings. Suboxone’s ability to reduce withdrawal-related distress contributes to decreased cravings.
- Long-Term Craving Management: As individuals progress in their recovery journey, they learn coping mechanisms and relapse prevention strategies, further contributing to reduced cravings over time.
Duration of Suboxone’s Blockade
The duration of Suboxone’s blockade largely depends on the half-life of its active ingredients, buprenorphine, and naloxone. Buprenorphine’s long half-life allows for sustained receptor occupation, extending the effects of Suboxone. Naloxone, although present to deter misuse, has a relatively short half-life and does not significantly impact the overall duration of Suboxone’s action.
Binding to Opioid Receptors
Buprenorphine’s high affinity for opioid receptors leads to strong and long-lasting binding. Once bound, it forms a stable connection, effectively blocking other opioids from attaching to these receptors. This blockade can last for several hours, providing a sustained effect against cravings and withdrawal.
Half-Life of Buprenorphine and Naloxone
- Buprenorphine’s Elimination Half-Life: Buprenorphine’s half-life ranges from 24 to 60 hours, depending on individual factors. This extended half-life contributes to the prolonged duration of Suboxone’s action.
- Naloxone’s Short Half-Life: Naloxone’s half-life is much shorter, typically around 1 to 2 hours. Although present to prevent misuse, naloxone’s impact on Suboxone’s overall duration is minimal.
Peak Effects and Tapering Off
After taking Suboxone, the effects gradually increase until reaching peak levels within a few hours. These peak effects are generally not as intense as those caused by full opioid agonists. As the effects wear off, individuals may experience a gradual decrease in Suboxone’s action, leading to a potential need for dose adjustments or tapering off the medication.
Peak Plasma Concentration
- Timing of Peak Effects: The peak plasma concentration of buprenorphine occurs within 1 to 4 hours after sublingual administration, resulting in the peak effects of Suboxone during this period.
- Steady-State Levels: With continued dosing, steady-state levels of buprenorphine are achieved, maintaining a relatively constant effect over time.
Tapering Strategies
- Gradual Reduction of Dosage: Tapering off Suboxone should be under medical supervision, with the dosage gradually decreased over time to minimize withdrawal symptoms and cravings.
- Monitoring for Withdrawal Symptoms: During the tapering process, individuals should be closely monitored for any signs of withdrawal or discomfort, allowing for appropriate adjustments to the tapering schedule.
Suboxone Formulations and Duration
There are different formulations of Suboxone available, each with its own characteristics that affect the duration of action. Sublingual tablets and films are the most commonly used formulations, while extended-release injectable formulations offer an alternative for some patients.
Sublingual Tablets
Suboxone sublingual tablets are placed under the tongue for absorption, allowing the active ingredients to enter the bloodstream directly. The tablets dissolve gradually, releasing the medication over time. The duration of action for sublingual tablets typically ranges from 24 to 72 hours, depending on the individual’s metabolism and dosage.
Administration Process
- Placement Under the Tongue: Sublingual tablets are specifically designed to be placed under the tongue, where they rapidly dissolve in saliva.
- Absorption through Sublingual Mucosa: Once dissolved, the medication is absorbed through the sublingual mucosa and directly enters the bloodstream, bypassing the digestive system.
Dissolving and Absorption
- Factors Affecting Dissolution: The rate of tablet dissolution can be influenced by factors such as saliva production and mouth dryness.
- Rate of Absorption: Absorption through the sublingual mucosa ensures a quicker onset of effects compared to oral ingestion.
Sublingual Films
Suboxone sublingual films offer a convenient alternative to tablets. The films are placed under the tongue, where they dissolve rapidly and deliver the medication. Due to the film’s thinness, the absorption process may be slightly faster than with tablets. The duration of action for sublingual films is comparable to that of sublingual tablets, typically lasting between 24 and 72 hours.
Advantages Over Tablets
- Ease of Use: Sublingual films are easy to handle and dissolve quickly, making them more convenient for some individuals.
- Consistent Dosage Release: The uniformity of the film’s composition ensures consistent dosage delivery.
Comparative Duration
- Similar Duration to Tablets: The duration of action for sublingual films is similar to that of sublingual tablets, as they contain the same active ingredients.
- Individual Variability: As with tablets, individual variability in metabolism and other factors can influence the duration of Suboxone’s effects when using films.
Injectable Formulations
Extended-release injectable formulations of Suboxone, such as Sublocade, provide an alternative for individuals who may prefer less frequent dosing. These formulations are administered via subcutaneous injection and can provide consistent effects over an extended period, typically lasting up to one month.
Extended-Release Injections
- Slow Release of Medication: The medication in extended-release injections is released gradually over time, providing continuous blockade of opioid receptors.
- Reduced Frequency of Administration: Extended-release injections eliminate the need for daily dosing, allowing individuals to focus more on their recovery journey.
Frequency of Administration
- Monthly Injections: Extended-release formulations are typically administered once a month, simplifying the dosing schedule and minimizing the risk of missed doses.
- Individually Tailored: The dosing frequency may vary based on individual response and treatment progress, ensuring personalized care.
Extended Use of Suboxone
Extended use of Suboxone refers to the longer-term treatment duration for opioid addiction. It is essential to understand the benefits and considerations associated with using Suboxone over an extended period to ensure effective and sustainable recovery.
Effects on Long-Term Opioid Use
Suboxone has shown positive outcomes when used as part of long-term treatment for opioid addiction. Extended use helps individuals maintain abstinence from opioids, reducing the risk of relapse and associated negative consequences. With ongoing support and therapy, individuals can develop essential life skills and coping mechanisms, contributing to lasting recovery.
Reduction of Cravings and Relapse
- Craving Management: Extended use of Suboxone allows for continuous management of cravings, which can persist even during the later stages of recovery.
- Preventing Relapse: Suboxone’s blockade effect helps prevent relapse by discouraging the use of opioids, even when faced with triggers or stressful situations.
Improved Social Functioning
- Enhanced Stability: Extended use of Suboxone provides stability and allows individuals to focus on rebuilding their lives and relationships.
- Engagement in Productive Activities: As individuals progress in recovery, they may be better able to engage in work, education, and other productive activities, leading to an improved quality of life.
Treatment Duration for Opioid Addiction
The appropriate treatment duration for opioid addiction with Suboxone can vary depending on individual needs and treatment progress. While some individuals may benefit from short-term use, others may require more extended treatment to achieve lasting recovery.
Short-Term vs. Long-Term Treatment Plans
- Short-Term Plans: Short-term Suboxone treatment may be appropriate for individuals with mild opioid use disorder or as part of a detoxification process.
- Long-Term Plans: Long-term treatment with Suboxone is often recommended for individuals with severe opioid use disorder or those at high risk of relapse.
Individualized Treatment Length
- Customized Approach: Healthcare providers tailor Suboxone treatment plans to suit each individual’s specific needs, taking into account factors such as the severity of addiction, past treatment history, and underlying medical conditions.
- Continual Assessment: Regular assessments help determine the ongoing effectiveness of Suboxone treatment and whether adjustments to the treatment plan are necessary.
Potential Risks of Prolonged Suboxone Use
While Suboxone can be a valuable tool in long-term recovery, there are potential risks associated with extended use. It is essential to address these risks and implement appropriate safeguards to ensure safe and effective treatment.
Physical Dependence and Withdrawal
- Dependency on Suboxone: Prolonged use of Suboxone can lead to physical dependence on the medication. As a result, individuals may experience withdrawal symptoms if they abruptly stop taking it.
- Tapering Off Safely: To avoid withdrawal, individuals should work with their healthcare provider to develop a gradual tapering plan when discontinuing Suboxone.
Psychological Effects
- Mood and Behavior: In some cases, individuals on long-term Suboxone treatment may experience changes in mood, behavior, or cognitive function. Addressing these issues through therapy and support is crucial for successful recovery.
- Psychological Dependence: While Suboxone is less likely to cause psychological dependence compared to full opioid agonists, it is essential to address any emotional reliance on the medication as part of the treatment process.
Addressing Risks through Medical Supervision
- Regular Monitoring and Assessments: Healthcare providers closely monitor individuals on extended Suboxone treatment to identify any potential risks or side effects.
- Individualized Treatment Plans: Customized treatment plans take into account the individual’s unique needs and adjust medication dosages and duration accordingly.
Managing Suboxone Treatment
Effectively managing Suboxone treatment is crucial to maximize its benefits and support long-term recovery. Medical supervision, individualized treatment plans, and supportive therapies are essential components of successful Suboxone treatment.
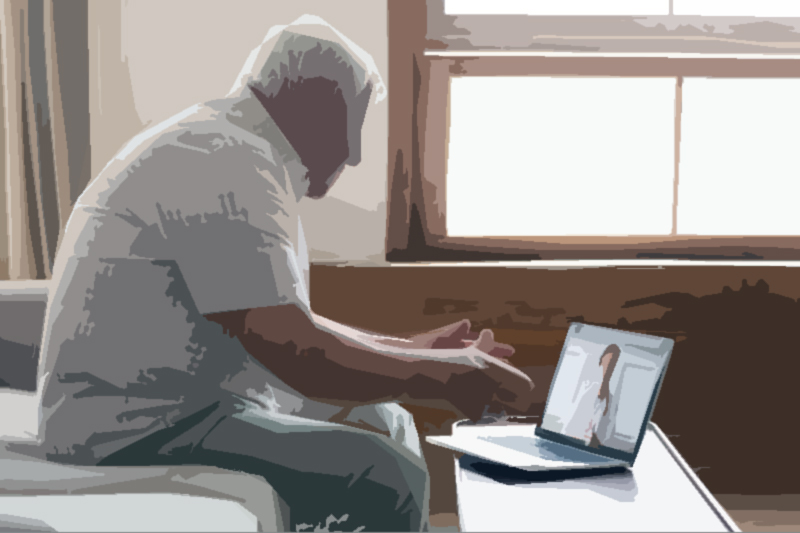
Medical Supervision and Individualized Plans
Suboxone treatment should always be carried out under the guidance of qualified healthcare professionals. A personalized treatment plan is developed based on each individual’s unique needs, medical history, and progress in recovery. Regular check-ups and monitoring help ensure that the treatment remains effective and safe.
Choosing the Right Treatment Setting
- Inpatient vs. Outpatient: The treatment setting may vary based on the severity of the addiction, the presence of co-occurring disorders, and the individual’s support network.
- Specialized Clinics: Some individuals may benefit from seeking treatment at specialized addiction clinics that offer comprehensive support services.
Personalized Dosing and Monitoring
- Adjusting Dosage: Individual responses to Suboxone can vary, and dosages may need to be adjusted to achieve optimal treatment outcomes.
- Monitoring for Side Effects: Regular monitoring helps identify and manage any potential side effects or adverse reactions to Suboxone.
Regular Assessment and Adjustments
Continual assessment of an individual’s progress and response to Suboxone treatment is essential for achieving positive outcomes. Healthcare providers regularly evaluate treatment effectiveness and may make necessary adjustments to dosage or other aspects of the treatment plan.
Monitoring Treatment Progress
- Physical and Psychological Well-Being: Regular check-ups help monitor an individual’s overall health and mental well-being throughout treatment.
- Adherence to Treatment Plan: Healthcare providers assess adherence to the treatment plan to ensure that Suboxone is being used effectively and appropriately.
Modifying Dosage and Duration
- Response to Treatment: Adjustments to Suboxone dosage or duration may be made based on an individual’s response to treatment and the presence of any side effects.
- Stages of Recovery: As individuals progress through different stages of recovery, treatment plans may need to be modified to address changing needs and goals.
Combining Suboxone with Other Therapies
Suboxone treatment is most effective when combined with other therapeutic approaches. Behavioral therapies, counseling, and support groups play a vital role in addressing the psychological and emotional aspects of addiction.
Behavioral Therapies
- Cognitive-Behavioral Therapy (CBT): CBT helps individuals identify and modify negative thought patterns and behaviors associated with drug use.
- Motivational Interviewing: This approach helps individuals find the internal motivation to change addictive behaviors and commit to recovery.
Support Groups
- 12-Step Programs: Participation in 12-step programs, such as Narcotics Anonymous (NA), provides peer support and a sense of community during recovery.
- Group Therapy: Group therapy sessions allow individuals to share their experiences, offer support, and learn from others in similar situations.
Addressing Co-Occurring Disorders
- Dual Diagnosis Treatment: For individuals with co-occurring mental health disorders, integrated treatment that addresses both addiction and mental health issues is crucial for long-term recovery.
- Comprehensive Care: Treating co-occurring disorders concurrently can enhance the effectiveness of Suboxone treatment and improve overall well-being.
Discontinuing Suboxone
At some point, individuals may consider discontinuing Suboxone treatment. However, the process of tapering off the medication requires careful planning and medical supervision to avoid potential withdrawal symptoms and relapse.
Tapering Off Safely
Tapering off Suboxone should be under the guidance of a healthcare provider to ensure a gradual reduction in dosage. Abruptly stopping Suboxone can lead to withdrawal symptoms and may increase the risk of relapse.
Gradual Reduction of Dosage
- Step-Down Approach: Tapering typically involves reducing the dosage incrementally over time until the individual is no longer taking Suboxone.
- Individualized Tapering Plans: Each person’s tapering plan is tailored to their specific needs, withdrawal symptoms, and progress in recovery.
Medical Guidance during Tapering
- Monitoring for Withdrawal Symptoms: Healthcare providers closely monitor individuals during the tapering process to manage any emerging withdrawal symptoms.
- Adjustments to the Tapering Schedule: If withdrawal symptoms become problematic, the tapering schedule may be adjusted to ensure a comfortable transition.
Withdrawal Symptoms and Duration
Withdrawal symptoms may occur when discontinuing Suboxone, especially if the tapering process is too rapid. The duration and intensity of withdrawal symptoms can vary based on individual factors.
Timeline of Withdrawal Symptoms
- Early Symptoms: Early withdrawal symptoms may start within a day or two after the last Suboxone dose and can include anxiety, sweating, and muscle aches.
- Peak Symptoms: The peak of withdrawal symptoms is typically reached within the first week and may include nausea, diarrhea, and insomnia.
- <strong
FAQs About How Long Suboxone Blocks Opioids
1. How long does Suboxone stay active in the body?
Suboxone’s duration of action can vary based on factors such as dosage, individual metabolism, and the specific formulation used. Generally, its effects can last between 24 to 72 hours.2. Can Suboxone block the effects of all opioids?
While Suboxone is effective in blocking many opioids, it may not completely block the effects of ultra-potent opioids such as fentanyl. However, its blockade effect can still reduce the risk of overdose.3. Is it safe to take Suboxone for an extended period?
Extended use of Suboxone under proper medical supervision can be safe and effective for managing opioid addiction. Medical providers regularly assess treatment progress to ensure its continued appropriateness.4. Can I switch from a sublingual tablet to a sublingual film formulation of Suboxone?
Yes, it is possible to switch between different Suboxone formulations, such as from a sublingual tablet to a sublingual film. However, any formulation change should be discussed with a healthcare provider first.5. What happens if I miss a dose of Suboxone?
If you miss a dose of Suboxone, take it as soon as you remember. However, if it is close to the time of your next scheduled dose, skip the missed dose and resume your regular dosing schedule. Do not take a double dose.6. Can I drink alcohol while taking Suboxone?
It is generally not recommended to consume alcohol while on Suboxone. Alcohol can increase the risk of sedation, respiratory depression, and other side effects when combined with Suboxone.7. Is Suboxone effective for everyone with opioid addiction?
While Suboxone can be highly effective for many individuals with opioid addiction, its suitability varies from person to person. Factors such as medical history, concurrent medications, and individual response should be considered.8. Can I stop taking Suboxone cold turkey?
Stopping Suboxone suddenly can lead to withdrawal symptoms and an increased risk of relapse. It is essential to work with a healthcare provider to develop a gradual tapering plan when discontinuing the medication.9. Does Suboxone cause drowsiness or impair cognitive function?
Suboxone may cause drowsiness and impair cognitive function, especially during the initial stages of treatment. It is crucial to avoid activities that require alertness until you know how Suboxone affects you.10. Can I use Suboxone as a sole treatment for opioid addiction?
While Suboxone is effective in managing opioid addiction, it is typically used as part of a comprehensive treatment approach that includes counseling, therapy, and support groups to address the psychological aspects of addiction.