The Ultimate Technical Guide to Bain Anesthesia Circuits7 min read
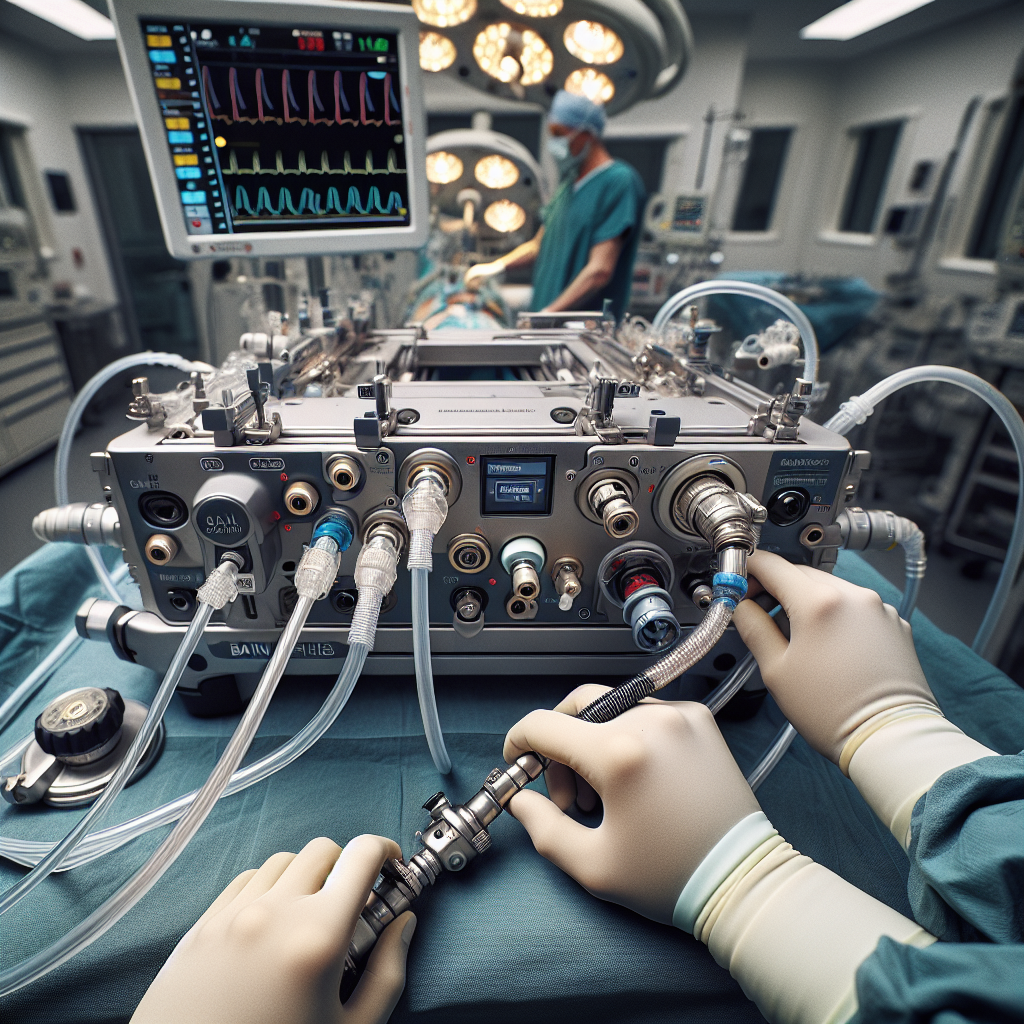
Are you looking for a comprehensive understanding of the Bain anesthesia circuit? This essential guide provides a detailed breakdown of its design, functionality, advantages, maintenance requirements, and clinical applications. Dive into the technical aspects and practical implementation of this widely used anesthesia system.
Understanding the Bain Circuit Design
The Bain anesthesia circuit, also known as the Bain coaxial circuit, is a compact and efficient system for delivering anesthetic gases to patients. Its unique design features a coaxial arrangement, where the fresh gas flow tube is located within the outer expiratory limb. This configuration allows for a lightweight and streamlined setup.
Components of the Bain Circuit
The Bain circuit consists of several key components:
- Fresh gas flow tube: Delivers fresh anesthetic gases from the machine to the patient
- Outer expiratory limb: Carries exhaled gases away from the patient
- Adjustable pressure-limiting (APL) valve: Regulates the pressure within the circuit
- Patient connection: Typically a mask or endotracheal tube
Coaxial Design Benefits
The coaxial arrangement of the Bain circuit offers several advantages:
- Reduced equipment dead space, minimizing rebreathing of exhaled gases
- Lightweight and compact design, enhancing portability and ease of use
- Simplified setup and maintenance compared to traditional circuits
By understanding the components and benefits of the Bain circuit’s design, clinicians can effectively utilize this system in anesthesia delivery.
Functionality and Gas Flow Dynamics
The Bain anesthesia circuit operates on the principle of continuous gas flow, ensuring a consistent supply of fresh anesthetic gases to the patient. Let’s explore the gas flow dynamics within the circuit.
Fresh Gas Flow
Fresh anesthetic gases enter the circuit through the inner fresh gas flow tube. The flow rate is controlled by the anesthesia machine and can be adjusted based on the patient’s requirements. The fresh gas flow mixes with the exhaled gases in the outer expiratory limb before reaching the patient.
Exhaled Gas Removal
As the patient exhales, the expired gases travel through the outer expiratory limb towards the adjustable pressure-limiting (APL) valve. The APL valve regulates the pressure within the circuit, allowing excess gases to escape while maintaining a desired level of positive end-expiratory pressure (PEEP).
Rebreathing Prevention
The Bain circuit’s design minimizes the rebreathing of exhaled gases by the patient. The high fresh gas flow rate and the placement of the fresh gas inlet near the patient connection ensure that the patient primarily inhales fresh anesthetic gases rather than exhaled gases.
By comprehending the gas flow dynamics, clinicians can optimize the Bain circuit’s performance and ensure proper anesthetic delivery to the patient.
Advantages of the Bain Circuit
The Bain anesthesia circuit offers several notable advantages that contribute to its widespread use in clinical settings. Let’s explore these benefits in detail.
Efficiency and Cost-Effectiveness
The Bain circuit’s simple design and minimal components make it a cost-effective choice for anesthesia delivery. Its efficiency in gas delivery and reduced equipment requirements contribute to overall cost savings in healthcare facilities.
Enhanced Patient Safety
The Bain circuit prioritizes patient safety through its design features. The coaxial arrangement minimizes dead space and reduces the risk of rebreathing exhaled gases. Additionally, the APL valve allows for precise control of circuit pressure, preventing barotrauma and ensuring optimal ventilation.
Versatility in Clinical Applications
The Bain circuit’s versatility makes it suitable for a wide range of clinical applications, including:
- General anesthesia for surgical procedures
- Sedation in intensive care units
- Anesthesia delivery in remote or emergency settings
Its adaptability to different patient populations and clinical scenarios enhances its utility in anesthesia practice.
By leveraging the advantages of the Bain circuit, clinicians can provide efficient, safe, and versatile anesthesia care to patients.
Maintenance and Troubleshooting
Proper maintenance and troubleshooting are essential to ensure the optimal performance and longevity of the Bain anesthesia circuit. Here are some key considerations:
Regular Inspection and Cleaning
Regular inspection of the Bain circuit components is crucial to identify any signs of wear, damage, or contamination. The circuit should be thoroughly cleaned and sterilized according to the manufacturer’s guidelines and institutional protocols. Particular attention should be given to the fresh gas flow tube and the APL valve to prevent blockages or leaks.
Leak Testing and Calibration
Leak testing should be performed before each use to ensure the integrity of the Bain circuit. Any leaks or disconnections should be promptly addressed to maintain proper gas delivery and patient safety. Regular calibration of the anesthesia machine and monitoring devices is also essential to ensure accurate readings and control.
Troubleshooting Common Issues
Common issues that may arise with the Bain circuit include:
- High airway pressures: Check for blockages, kinks, or herniation of the reservoir bag
- Inadequate gas flow: Verify the fresh gas flow settings and check for leaks
- APL valve malfunction: Inspect the valve for damage or obstruction and replace if necessary
Prompt identification and resolution of these issues are essential to maintain the circuit’s functionality and ensure uninterrupted anesthesia delivery.
By implementing a robust maintenance and troubleshooting protocol, clinicians can optimize the performance of the Bain anesthesia circuit and provide safe and reliable anesthesia care.
Clinical Considerations and Best Practices
When using the Bain anesthesia circuit in clinical practice, several considerations and best practices should be followed to ensure optimal patient care and safety.
Patient Selection and Monitoring
Careful patient selection is crucial when using the Bain circuit. Factors such as the patient’s age, weight, respiratory status, and comorbidities should be considered. Continuous monitoring of vital signs, including oxygenation, ventilation, and hemodynamics, is essential to detect and address any adverse events promptly.
Anesthetic Agent Selection and Dosing
The choice of anesthetic agents and their dosing should be tailored to the individual patient’s needs and the specific surgical procedure. The Bain circuit’s efficiency in gas delivery allows for precise control of anesthetic depth. However, clinicians must be vigilant in monitoring the patient’s response and adjusting the anesthetic concentration accordingly.
Infection Control Measures
Strict infection control measures should be implemented when using the Bain circuit. This includes the use of disposable or thoroughly sterilized components, proper hand hygiene, and adherence to aseptic techniques. The circuit should be replaced or sterilized between patients to minimize the risk of cross-contamination.
By adhering to these clinical considerations and best practices, clinicians can optimize patient safety and outcomes when using the Bain anesthesia circuit.
Frequently Asked Questions
What is the main advantage of the Bain circuit over other anesthesia circuits?
The main advantage of the Bain circuit is its compact and lightweight design, which allows for improved portability and ease of use. The coaxial arrangement of the fresh gas flow tube within the outer expiratory limb reduces equipment dead space and minimizes the risk of rebreathing exhaled gases.
How does the Bain circuit differ from Mapleson circuits?
The Bain circuit is a modified version of the Mapleson D circuit. While Mapleson circuits have separate inspiratory and expiratory limbs, the Bain circuit combines them into a coaxial arrangement. This modification simplifies the circuit design and reduces the overall size and weight of the system.
Can the Bain circuit be used for pediatric patients?
Yes, the Bain circuit can be used for pediatric patients with appropriate modifications. The circuit can be adapted with smaller diameter tubing and connectors to accommodate the reduced tidal volumes and respiratory rates of pediatric patients. However, careful monitoring and adjustment of fresh gas flow rates are essential to prevent excessive airway pressures and ensure adequate ventilation.
How often should the Bain circuit be replaced?
The frequency of replacing the Bain circuit depends on the manufacturer’s recommendations and institutional protocols. Generally, the circuit should be replaced between patients to minimize the risk of cross-contamination. Additionally, any signs of wear, damage, or contamination should prompt immediate replacement to ensure optimal performance and patient safety.
Conclusion
The Bain anesthesia circuit is a reliable and efficient system for delivering anesthetic gases to patients. Its unique coaxial design offers advantages such as reduced equipment dead space, improved portability, and simplified setup. By understanding the circuit’s functionality, gas flow dynamics, and clinical considerations, clinicians can effectively utilize the Bain circuit in a wide range of anesthesia applications.
This comprehensive technical guide has provided insights into the design, advantages, maintenance, and best practices associated with the Bain anesthesia circuit. By leveraging this knowledge, clinicians can optimize patient safety, enhance anesthesia delivery, and achieve successful outcomes in their practice.