Are antibiotics and anesthesia a dynamic duo or a conflicting combination? Delve into the intricate relationship between these two crucial elements of medical care. In this article, we explore how antibiotics and anesthesia might interact, offering insights into the potential implications for patients undergoing surgery. From the mechanisms behind antibiotics’ action to the nuances of anesthesia administration, discover the key factors that healthcare professionals consider when navigating this complex interplay.
- Key Points:
- Understanding the role of antibiotics in combating infections
- Exploring the significance of anesthesia for safe and comfortable surgeries
- Possible interactions that could affect anesthesia efficacy
- Mechanisms through which antibiotics might impact anesthetic agents
- Factors influencing the antibiotics-anesthesia relationship
- Guidelines for healthcare practitioners to manage potential interactions
The Mechanics of Antibiotics and Anesthesia
In the realm of medicine, antibiotics play the role of infection fighters, while anesthesia ensures patients undergo procedures without pain or consciousness. Antibiotics function by targeting specific processes in bacteria, inhibiting their growth or causing cell death. On the other hand, anesthesia agents act on the nervous system to induce temporary unconsciousness, analgesia, and muscle relaxation.
Potential Interplay: Antibiotics and Anesthesia
When antibiotics and anesthesia coexist in a patient’s body, there’s potential for interaction due to their impact on physiological pathways. Some antibiotics, notably those affecting liver enzymes, can alter the metabolism of anesthesia agents. This alteration might lead to unexpected fluctuations in anesthetic depth, potentially affecting patient outcomes during surgery.
The Impact of Enzyme Activity
Certain antibiotics can induce or inhibit specific enzymes responsible for metabolizing anesthesia drugs. Enzyme induction might accelerate the breakdown of anesthetics, resulting in shortened effects. Conversely, enzyme inhibition could prolong the presence of anesthetic agents in the body, potentially leading to prolonged unconsciousness or delayed emergence.
- Considerations:
- Which antibiotic classes are more likely to induce or inhibit enzymes?
- How does enzyme modulation vary across different anesthesia agents?
- What precautions can anesthesiologists take to mitigate enzyme-related interactions?
Neurotransmitter Modulation
Some antibiotics might impact neurotransmitter pathways in the brain, potentially influencing the response to anesthesia agents. For instance, alterations in neurotransmitter levels could affect the onset and duration of anesthesia-induced unconsciousness. Anesthesiologists carefully assess these potential interactions to ensure precise control over the anesthesia experience.
- Exploration:
- Which neurotransmitters are most crucial for anesthesia induction?
- How might antibiotics disrupt the delicate balance of neurotransmitter signaling?
- What steps can be taken to minimize unpredictable anesthesia effects?
Antibiotic Classes and Their Varied Effects on Anesthesia
Diverse Antibiotic Families
Penicillins: Unlikely to Cause Major Anesthetic Interactions
- Commonly used for bacterial infections
- Minimal impact on liver enzymes metabolizing anesthesia agents
Macrolides: Potential for Enzyme Inhibition
- Used against respiratory and skin infections
- May inhibit enzymes affecting anesthesia agent breakdown
Patient-Specific Factors in Antibiotic-Anesthesia Interaction
Metabolism and Drug Interactions
Genetic Variability in Enzyme Activity
- Impact of genetic factors on enzyme induction and inhibition
- Personalized anesthesia dosing to accommodate genetic variations
Drug Interaction Networks
- How antibiotic-anesthesia interaction fits into broader drug interactions
- Cautious prescribing to avoid compounded drug effects
Navigating Antibiotics and Anesthesia: Practical Guidelines
Preoperative Screening Protocols
Comprehensive Patient Assessment
- Evaluating antibiotic history and potential impact on anesthesia
- Identifying risk factors for enzyme-related interactions
Collaboration Among Medical Teams
- Open communication between anesthesiologists and infectious disease specialists
- Shared decision-making based on antibiotic regimen and surgery plan
Real Cases: Antibiotic-Anesthesia Complications
Unexpected Anesthetic Prolongation
Case Study: Quinolones and Enzyme Inhibition
- Quinolone antibiotics’ potential to prolong anesthesia effects
- Clinical implications for anesthetic dosage adjustments
Case Study: Anesthesia Depth Alteration
- Impact of certain antibiotics on neurotransmitter balance
- Ensuring precise control over anesthesia depth
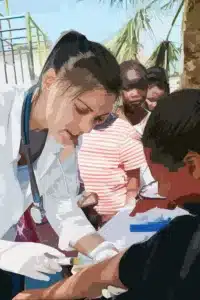
Antibiotics, Anesthesia, and Pediatric Patients
Unique Considerations for Children
Developing Metabolic Enzymes in Pediatric Patients
- Age-related variations in enzyme activity and drug metabolism
- Special precautions when administering antibiotics and anesthesia
Choosing Appropriate Antibiotics for Pediatric Surgery
- Selection criteria to minimize potential interactions
- Ensuring safety and efficacy in young patients
Research Frontiers: Antibiotics and Anesthesia
Emerging Studies on Mechanisms
Neuroinflammation and Anesthetic Response
- Exploring links between antibiotics, inflammation, and anesthesia effects
- Implications for patient selection and tailored anesthesia plans
Genetic Markers Predicting Interaction Risks
- Advancements in genetic testing for personalized anesthesia strategies
- Potential to mitigate unexpected antibiotic-anesthesia interactions
Safe Practice: Minimizing Risks of Antibiotic-Anesthesia Interaction
Integrated Medical Approaches
Optimal Timing of Antibiotic Administration
- Aligning antibiotic dosing with anesthesia induction
- Minimizing potential delays in surgery due to antibiotic effects
Monitoring and Adaptation
- Real-time assessment of anesthesia depth and patient response
- Immediate adjustments to anesthesia plan in case of unexpected effects
Antibiotic Prophylaxis and Anesthesia in Surgery
Rationale for Antibiotic Prophylaxis
Reducing Surgical Site Infections
- Administration of antibiotics before surgery to prevent postoperative infections
- Enhancing patient outcomes and minimizing healthcare costs
Interplay with Anesthesia
- Choosing antibiotics with minimal impact on anesthesia agents
- Coordinated administration to maximize both infection prevention and anesthesia efficacy
Specialty Procedures: Antibiotics, Anesthesia, and Cardiovascular Surgeries
Complex Considerations in Cardiovascular Cases
Antibiotics for Endocarditis Prophylaxis
- Special antibiotics administered before cardiac surgeries to prevent endocarditis
- Effects of these antibiotics on anesthesia dynamics
Cardiopulmonary Bypass and Anesthesia Interaction
- Antibiotics’ potential impact on coagulation factors during cardiac procedures
- Anesthesia strategies to mitigate potential bleeding risks
Antibiotics and Regional Anesthesia: A Balancing Act
Localized Anesthesia and Antibiotic Regimens
Spinal and Epidural Anesthesia
- Interactions between antibiotics and anesthetic agents in the spinal or epidural space
- Ensuring anesthetic potency and patient comfort
Peripheral Nerve Blocks
- Optimal timing of antibiotic administration in relation to nerve block procedures
- Minimizing the risk of disrupted anesthetic effects
Challenges of Antibiotic-Induced GI Disturbances and Anesthesia
Gastrointestinal Effects of Antibiotics
Antibiotic-Associated Diarrhea and Anesthesia
- How antibiotics might affect the gut and gastrointestinal motility
- Managing potential complications during anesthesia induction
Implications for Anesthetic Agents
- Choosing anesthesia agents that align with potential GI disturbances
- Adjusting anesthesia plan based on patient’s gastrointestinal health
Postoperative Care: Antibiotics, Anesthesia, and Recovery
Recovery Challenges and Considerations
Delayed Emergence and Antibiotic Presence
- How prolonged antibiotic effects can impact anesthesia recovery
- Strategies for optimizing emergence and patient wake-up
Pain Management and Antibiotic-Anesthetic Interaction
- Possible interactions between pain medications, antibiotics, and anesthesia
- Personalizing pain relief strategies for patients on antibiotics
Antibiotics, Anesthesia, and Elderly Patients
Geriatric Population and Drug Interactions
Age-Related Changes in Enzyme Activity
- How aging affects enzyme function and drug metabolism
- Anticipating potential antibiotic-anesthesia interactions in older patients
Polypharmacy and Anesthesia Complications
- Considering multiple medications in elderly patients on antibiotics
- Addressing heightened potential for drug interactions during anesthesia
Advancing Knowledge: Ongoing Antibiotic-Anesthesia Research
Emerging Interdisciplinary Studies
Pharmacogenomics and Tailored Anesthesia
- Exploring genetic variations impacting antibiotic-anesthesia interactions
- Customizing anesthesia plans based on individual genetic profiles
Neurological Implications of Long-Term Antibiotics
- Investigating potential cognitive effects of extended antibiotic use on anesthesia response
- Considering long-term patient outcomes beyond the surgical event
Enhancing Patient Education: Antibiotics, Anesthesia, and Informed Consent
Empowering Patients with Information
Understanding Potential Effects on Anesthesia Experience
- Importance of transparent communication between healthcare providers and patients
- Addressing patient concerns about antibiotic-anesthesia interactions
Emphasizing Informed Consent
- Ensuring patients are aware of potential risks and benefits of antibiotics and anesthesia
- Allowing patients to make informed decisions about their medical care
Crossroads of Pharmacology: Antibiotics and Anesthesia Pharmacodynamics
Shared Pharmacological Principles
Overlap in Neurotransmitter Regulation
- Similar neurotransmitter pathways targeted by both antibiotics and anesthesia
- Potential amplification of effects or unintended interference
Drug Synergy and Impact on Patient Response
- Concurrent administration’s potential to enhance or alter anesthesia’s effects
- Adjusting anesthesia doses for patients on specific antibiotic regimens
Antibiotics and Local Anesthetics: Implications for Dental Procedures
Dentistry and the Antibiotic-Anesthesia Landscape
Antibiotics in Preventive Dental Procedures
- Prophylactic antibiotic use in dental surgeries and anesthesia considerations
- Optimizing anesthesia delivery while maintaining infection prevention
Local Anesthetics and Antibiotic Selection
- Choosing antibiotics with minimal interference with dental local anesthetics
- Ensuring pain-free procedures without compromising infection control
Antibiotics and Anesthesia: Psychological Considerations
Patient Anxiety and Anesthetic Response
The Anxiety-Aware Anesthesia Approach
- Addressing patient anxiety and its potential impact on anesthesia efficacy
- Strategies to mitigate anxiety-related interference during anesthesia
Antibiotics’ Influence on Psychological State
- Exploring antibiotic effects on mood and emotional well-being
- Collaborative management of psychological and physiological aspects
Antibiotic-Induced Allergic Reactions and Anesthesia
Unraveling Allergic Responses
Anesthesia Management in Allergic Patients
- Antibiotic allergies’ potential influence on anesthesia agent choices
- Preventing allergic reactions during surgery through tailored anesthesia strategies
Emergency Preparedness and Rapid Response
- Preparing for potential allergic reactions and anesthetic complications
- Efficiently addressing adverse events while ensuring patient safety
Collaborative Research: Antibiotics, Anesthesia, and Medical Ethics
Exploring Ethical Dimensions
Informed Consent and Dual Impact
- Ensuring patients comprehend both antibiotic and anesthesia implications
- Ethical responsibility of healthcare providers in fostering patient understanding
Ethical Considerations in Research
- Conducting studies to enhance knowledge while prioritizing patient safety
- Maintaining ethical standards in investigating antibiotic-anesthesia interactions
Future Prospects: Antibiotics and Precision Anesthesia
Towards Personalized Anesthesia Approaches
Integration of Patient Data for Tailored Anesthesia
- Incorporating antibiotic history, genetics, and more into anesthesia plans
- Utilizing technology to optimize patient-specific anesthesia administration
Advancements in Drug Design and Delivery
- Developing anesthesia agents with reduced susceptibility to antibiotic interactions
- Improving patient outcomes through innovation in drug formulations
Antibiotics and Anesthesia: Bridging the Knowledge Gap
Constant Evolution of Medical Understanding
In the ever-evolving landscape of medicine, the relationship between antibiotics and anesthesia remains an area of ongoing research and discovery. Healthcare professionals continuously strive to uncover the nuances of their interaction to enhance patient care.
Interdisciplinary Collaboration for Holistic Care
- Integration of infectious disease specialists, anesthesiologists, and surgeons
- Combining diverse expertise to optimize surgical outcomes and patient well-being
Research Pathways and Future Insights
- Investigating lesser-known antibiotic-anesthesia interactions
- Unraveling the impact of new antibiotic formulations on anesthesia agents
The Road Ahead: Optimizing Antibiotic-Anesthesia Integration
Maximizing Patient Safety
As medical knowledge deepens, practitioners strive to ensure that patients experience the best possible outcomes. By refining antibiotic and anesthesia protocols, medical teams can minimize risks and maximize safety during surgical procedures.
Customized Anesthetic Approaches
- Tailoring anesthesia plans based on individual patient factors and antibiotic regimens
- Advancing personalized medicine through precise dosage adjustments
Pioneering Evidence-Based Practices
- Continuing to base medical decisions on the latest research and clinical evidence
- Constantly evolving practices to reflect the changing landscape of medicine
Conclusion: The Art and Science of Antibiotics and Anesthesia
Harmonizing Two Essential Components of Care
The intricate interplay between antibiotics and anesthesia is both an art and a science. As medical professionals navigate this complex landscape, they exemplify the delicate balance between fighting infection and ensuring safe surgical experiences for patients.
Empowering Patients and Practitioners
- Educating patients about potential interactions and anesthesia options
- Equipping medical teams with knowledge to make informed decisions
Continuous Advancements for Enhanced Healthcare
- Anticipating ongoing research breakthroughs for improved patient outcomes
- Harnessing medical innovations to shape the future of antibiotic-anesthesia integration
Frequently Asked Questions (FAQs)
FAQ 1: Can antibiotics affect the effectiveness of anesthesia?
Answer: Yes, certain antibiotics can interact with anesthesia agents and potentially alter their effectiveness. The impact depends on factors such as the specific antibiotic class, patient health, and anesthesia type.
FAQ 2: Are there antibiotics that are less likely to interfere with anesthesia?
Answer: Yes, some antibiotics, like penicillins, are generally considered to have minimal impact on anesthesia agents. However, it’s essential to consider individual patient factors and consult medical professionals for personalized recommendations.
FAQ 3: How do antibiotics influence enzyme activity relevant to anesthesia?
Answer: Some antibiotics can induce or inhibit enzymes responsible for metabolizing anesthesia drugs. Enzyme induction may lead to faster breakdown of anesthetics, while inhibition could prolong their effects.
FAQ 4: What role does patient health play in antibiotic-anesthesia interaction?
Answer: Patient health and medical history significantly influence this interaction. Factors such as metabolism, immune response, and existing conditions can impact how antibiotics and anesthesia agents interact within the body.
FAQ 5: Can antibiotics alter the onset and duration of anesthesia?
Answer: Yes, antibiotics might influence neurotransmitter pathways in the brain, potentially affecting the onset and duration of anesthesia-induced unconsciousness. Close monitoring and adjustment are necessary in such cases.
FAQ 6: How can medical teams mitigate antibiotic-anesthesia complications?
Answer: Collaborative efforts between anesthesiologists, surgeons, and infectious disease specialists are crucial. Transparent communication, patient assessment, and customized anesthesia plans based on antibiotic regimens can help manage potential interactions.
FAQ 7: Are there antibiotics that should be avoided before surgery?
Answer: Some antibiotics, particularly those affecting enzyme activity, might require careful consideration before surgery. This is to prevent unintended interactions with anesthesia agents that could affect patient outcomes.
FAQ 8: What should patients undergoing surgery know about antibiotics and anesthesia?
Answer: Patients should be aware of potential interactions between antibiotics and anesthesia. They should communicate their antibiotic history to medical teams, ask questions, and follow medical advice to ensure a safe surgical experience.
FAQ 9: Can elderly patients be more susceptible to antibiotic-anesthesia interactions?
Answer: Yes, aging can impact enzyme activity and drug metabolism, potentially making elderly patients more vulnerable to interactions between antibiotics and anesthesia. Careful assessment and personalized anesthesia plans are essential.
FAQ 10: What does ongoing research reveal about antibiotics and anesthesia?
Answer: Ongoing research sheds light on genetic factors, neurotransmitter regulation, and neurological implications of this interaction. The aim is to enhance patient safety and refine anesthesia strategies based on evolving scientific insights.