Naloxone, the opioid overdose reversal agent, has garnered immense attention for its crucial role in saving lives amid the opioid crisis. But what exactly is naloxone, and is it an opioid itself? In this article, we delve into the depths of naloxone’s pharmacology and its relationship with opioids. Prepare to uncover the fascinating science behind this life-saving antidote.
- Understanding Naloxone: Learn about the chemical properties, origin, and medical uses of naloxone.
- How Naloxone Works: Discover how naloxone interacts with opioid receptors and effectively reverses opioid overdose.
- Naloxone and Opioid Overdose: Explore the pivotal role of naloxone as an emergency tool in opioid overdose situations.
- Is Naloxone Itself an Opioid? Gain insights into naloxone’s distinct pharmacological classification and its effects on opioid receptors.
- Benefits and Limitations of Naloxone: Delve into the advantages and considerations surrounding naloxone’s use.
- Naloxone Access and Availability: Understand the legal aspects and efforts to increase naloxone accessibility.
Naloxone: An Essential Weapon Against Opioid Overdose
Naloxone, commonly known by the brand name Narcan, is a potent opioid receptor antagonist. This means it binds to opioid receptors in the brain, displacing any opioids that may be present, and rapidly reverses the life-threatening effects of opioid overdose, particularly respiratory depression. It is a critical tool for first responders, healthcare professionals, and even laypeople in emergency situations where opioid overdose is suspected.
The chemical structure of naloxone enables it to compete with opioids for binding to the mu, delta, and kappa opioid receptors in the brain. By outcompeting opioids, naloxone effectively blocks their actions, thereby restoring normal breathing and preventing the overdose’s potentially fatal consequences.
Naloxone and Opioid Overdose: A Race Against Time
When someone experiences an opioid overdose, time is of the essence. Opioids can cause severe respiratory depression, leading to a lack of oxygen in the body. Without intervention, this can result in brain damage or death. This is where naloxone plays a crucial role.
Naloxone is available in various forms, including injectable formulations and nasal sprays. Its rapid onset of action makes it a life-saving antidote. When administered promptly, naloxone can reverse opioid overdose effects within minutes. However, it’s essential to remember that naloxone’s effects are temporary, and the person still needs medical attention after administration.
Using Naloxone: A Step-by-Step Guide
- Assess the Situation: If you suspect someone has overdosed on opioids, call for emergency medical help immediately.
- Administer Naloxone: If naloxone is available, follow the specific instructions for the given formulation (e.g., intramuscular injection or nasal spray). Don’t hesitate to administer it, as naloxone is safe even if opioids are not present.
- Observe the Response: Once naloxone is given, closely monitor the individual’s response. Breathing should improve within a few minutes, but be prepared to administer additional doses if needed.
- Seek Medical Attention: Remember that naloxone is not a substitute for professional medical care. Even if the person appears to have recovered, they should still be taken to a hospital for evaluation and treatment.
- Dispose of Naloxone Safely: If the naloxone was administered using an auto-injector, dispose of it responsibly according to local guidelines.
The Role of Naloxone in Combating the Opioid Crisis
Empowering Communities with Naloxone Access
Naloxone distribution programs have become a vital component of harm reduction efforts. Many communities now provide naloxone kits to individuals at risk of opioid overdose or those close to individuals struggling with opioid use disorder. These initiatives aim to empower communities to respond promptly to overdose emergencies, potentially saving lives and reducing the devastating impact of the opioid crisis.
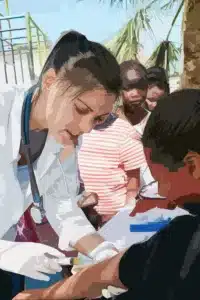
Community-Based Naloxone Training
- Education on Opioid Overdose Recognition: Naloxone training sessions focus on teaching individuals how to recognize the signs of an opioid overdose, such as slowed or shallow breathing and unresponsiveness.
- Proper Naloxone Administration Techniques: Participants learn how to use naloxone effectively, whether through intramuscular injection or nasal spray, ensuring that the antidote reaches the opioid receptors efficiently.
- Addressing Stigma and Misconceptions: Naloxone training programs also aim to dispel stigma and fear surrounding opioid use and naloxone, promoting a compassionate approach to supporting individuals dealing with addiction.
Naloxone in the Hands of First Responders
Integration into Emergency Medical Services
In many regions, emergency medical services (EMS) personnel are equipped with naloxone as part of their standard protocol. This integration ensures that naloxone is readily available at the scene of suspected opioid overdoses, providing a rapid and professional response to potentially life-threatening situations.
EMS Naloxone Administration Protocols
- Training for EMS Personnel: EMS providers undergo rigorous training in recognizing opioid overdose, determining the appropriate naloxone dosage, and administering it safely and effectively.
- Coordinating with Other Healthcare Providers: EMS personnel collaborate with hospitals and healthcare facilities to ensure a seamless continuum of care for individuals who receive naloxone treatment.
- Data Collection and Monitoring: EMS agencies often track naloxone administrations to identify overdose trends and assess the impact of naloxone distribution efforts on their communities.
Naloxone: A Bridge to Recovery
Supporting Opioid Use Disorder Treatment
Naloxone not only saves lives during overdose emergencies but also plays a role in supporting individuals on their path to recovery from opioid use disorder. By reversing overdoses, naloxone provides a second chance for individuals to seek treatment and address the underlying causes of their opioid dependence.
Naloxone as a Harm Reduction Strategy
- Reducing Fatalities and Morbidity: By preventing overdose deaths, naloxone offers the opportunity for individuals to seek treatment and engage in recovery-oriented care, potentially reducing long-term health complications.
- Building Trust and Engagement: Distributing naloxone fosters trust between healthcare providers and individuals struggling with opioid use, creating a gateway to connect them with treatment resources.
- Connecting to Support Services: Naloxone distribution programs often link individuals to substance use disorder treatment facilities, counseling services, and harm reduction support networks.
Naloxone and Law Enforcement Agencies
Equipping Officers with Naloxone
In recent years, the opioid crisis has prompted many law enforcement agencies to equip their officers with naloxone. This move recognizes that officers are often the first on the scene in overdose emergencies and can play a vital role in saving lives by administering naloxone promptly.
Training and Implementation Challenges
- Training Police Officers: Law enforcement personnel receive specialized training on recognizing opioid overdose symptoms and administering naloxone effectively.
- Policy Development and Adoption: Implementing naloxone programs in law enforcement requires developing comprehensive policies and protocols to ensure the proper use and documentation of naloxone administrations.
- Community Impact and Public Perception: Equipping officers with naloxone can positively impact community relations and demonstrate a commitment to public health and safety.
Naloxone and Harm Reduction Organizations
Frontline Advocates for Naloxone Access
Harm reduction organizations have been at the forefront of advocating for naloxone access and distribution. These grassroots initiatives aim to reduce the negative consequences of drug use by promoting health and safety measures, such as naloxone distribution and syringe exchange programs.
Overcoming Barriers to Naloxone Distribution
- Advocacy and Policy Change: Harm reduction organizations work tirelessly to advocate for policy changes that remove barriers to naloxone access and increase funding for distribution programs.
- Outreach and Education: These organizations engage with vulnerable populations to provide education on naloxone use, encourage safer drug use practices, and foster community support networks.
- Challenges in Stigmatized Environments: Naloxone distribution efforts in areas with high stigma surrounding substance use face unique challenges, requiring innovative strategies to reach those most in need.
Naloxone for At-Home Use
Prescribing Naloxone to Patients on Opioid Medications
Healthcare providers are increasingly prescribing naloxone to patients who are on long-term opioid medications, especially those at a higher risk of opioid overdose. This practice is part of a broader effort to enhance patient safety and mitigate the risk of unintentional overdoses.
Promoting Patient Education and Empowerment
- Encouraging Open Conversations: Healthcare providers engage in honest discussions with patients about the risks of opioid medications and the importance of having naloxone on hand, even for prescribed use.
- Integration into Pain Management Plans: Naloxone is now considered a standard component of pain management plans for patients on high-dose or long-term opioid therapy.
- Training Caregivers and Family Members: Patients are encouraged to involve their caregivers and family members in naloxone training to ensure a rapid response in case of an emergency.
Naloxone for Veterinary Use
Protecting Working Animals from Opioid Exposure
In some cases, naloxone is used in veterinary medicine to safeguard working animals, such as police or detection dogs, from accidental opioid exposure. These animals can be exposed to opioids during drug detection operations or when searching for illegal substances.
Veterinarian Training and Preparedness
- Recognition of Opioid Exposure Symptoms: Veterinarians and animal handlers receive training on identifying signs of opioid exposure in working animals, as symptoms may differ from those seen in humans.
- Administering Naloxone to Animals: Veterinary professionals are taught the appropriate dosage and administration methods of naloxone for animals, as it may differ from human protocols.
- Proactive Measures and Safety Protocols: Organizations that use working animals implement safety protocols to minimize the risk of opioid exposure and ensure immediate access to naloxone when needed.
Naloxone and Pediatric Considerations
Promoting Safe Use in Children
While naloxone is a life-saving medication, its use in pediatric populations requires special considerations due to differences in physiology and weight-based dosing. Healthcare providers must carefully assess the risks and benefits when administering naloxone to children.
Pediatric Naloxone Administration Guidelines
- Age and Weight-Based Dosing: Pediatric naloxone dosing is tailored to the child’s age, weight, and medical condition, ensuring optimal effectiveness while minimizing potential adverse effects.
- Training for Caregivers and School Personnel: Parents, guardians, and school staff may receive training in recognizing opioid overdose symptoms in children and administering naloxone if needed.
- Addressing Parental Concerns: Healthcare providers engage in open conversations with parents or guardians about naloxone’s role in emergency situations, alleviating any anxieties or misconceptions.
Naloxone and Opioid Tolerance
Challenges in Overdose Reversal for Chronic Opioid Users
Individuals with chronic opioid use may develop tolerance over time, requiring higher doses of opioids to achieve the same effects. As a result, reversing opioid overdose in this population can be more challenging and may require larger amounts of naloxone.
Managing Overdoses in Tolerant Individuals
- Intramuscular vs. Intravenous Naloxone: Healthcare providers may opt for intravenous naloxone administration in cases of opioid-tolerant individuals due to its rapid onset of action.
- Continuous Monitoring and Reversal: In some cases, multiple doses of naloxone and extended monitoring are necessary to completely reverse an opioid overdose in individuals with high opioid tolerance.
- Multimodal Approach to Overdose Treatment: Overdose cases involving opioid-tolerant individuals may require additional interventions, such as assisted ventilation or other supportive measures, to ensure adequate respiratory function.
Combating Naloxone Stigma
Changing Perceptions and Misunderstandings
Despite its life-saving potential, naloxone can face stigma and misconceptions, leading to hesitancy in its use or distribution. Dispelling these myths is essential in ensuring naloxone is widely accepted and accessible.
Educational Initiatives and Public Awareness
- Media and Information Campaigns: Educational campaigns, both online and offline, aim to provide accurate information about naloxone, its safety, and its importance in overdose response.
- Training for Healthcare Providers: Healthcare professionals receive training on addressing naloxone stigma and effectively communicating its benefits to patients and their families.
- Community Testimonials and Success Stories: Sharing success stories of naloxone administration and lives saved helps humanize its impact and combat negative perceptions.
Future Developments in Naloxone Formulations
Advancing Delivery Methods and Effectiveness
As technology and research progress, scientists are exploring innovative formulations and delivery methods to enhance naloxone’s effectiveness and ease of use.
Novel Naloxone Formulations Under Investigation
- Long-Acting Naloxone: Researchers are exploring formulations that provide extended duration of action, reducing the need for frequent redosing and improving compliance.
- Intranasal Spray Enhancements: Efforts are underway to improve the absorption and bioavailability of intranasal naloxone sprays, making them more efficient in overdose reversal.
- Auto-Injectors and Novel Devices: User-friendly auto-injectors and other innovative devices aim to simplify naloxone administration, making it accessible to a broader range of individuals.
Naloxone in the Global Context
Addressing Overdose Crises Worldwide
The opioid epidemic is not limited to one country or region; it is a global health challenge. Naloxone distribution efforts have expanded internationally to combat overdose crises and promote harm reduction strategies.
Challenges and Successes in Global Naloxone Programs
- Varied Legal and Regulatory Environments: Naloxone distribution faces different legal and regulatory challenges in various countries, impacting accessibility and implementation.
- Cultural Perceptions and Stigma: Cultural attitudes toward drug use and naloxone can influence its acceptance and effectiveness in different societies.
- International Collaboration and Knowledge Sharing: Global initiatives encourage the exchange of best practices and lessons learned between countries to optimize naloxone distribution and overdose response strategies.
Naloxone and Emergency Department Protocols
Integrating Naloxone into Emergency Care
Emergency departments play a crucial role in managing opioid overdoses and providing timely naloxone administration. Protocols have been developed to ensure a systematic and efficient approach to overdose treatment.
Emergency Department Naloxone Guidelines
- Rapid Triage and Assessment: Patients presenting with suspected opioid overdose are rapidly assessed, and naloxone administration is prioritized to address respiratory depression promptly.
- Titration and Monitoring: Emergency departments carefully monitor patients after naloxone administration, adjusting dosages as needed to maintain respiratory function without precipitating withdrawal symptoms.
- Discharge Planning and Follow-Up: Patients who receive naloxone in the emergency department are offered further support, including referral to addiction treatment programs, counseling services, and harm reduction resources.
Naloxone’s Impact on Mortality Rates
Examining the Evidence
Studies have demonstrated the significant impact of naloxone distribution on reducing opioid overdose-related mortality rates. Access to naloxone has been associated with fewer deaths and improved survival outcomes.
Evidence-Based Findings on Naloxone Efficacy
- Community-Level Interventions: Naloxone distribution programs implemented at the community level have been linked to decreased mortality rates and increased bystander intervention in overdose situations.
- Naloxone Co-Prescribing Initiatives: Prescribing naloxone alongside opioid medications has been shown to reduce fatal overdose rates among patients on long-term opioid therapy.
- Public Health Impact: Naloxone’s widespread availability has contributed to a positive public health impact by saving lives and increasing awareness of overdose risks.
Empowering Individuals Through Naloxone Training
Creating a Naloxone-Ready Society
Efforts to expand naloxone access extend beyond medical professionals and first responders. Training laypeople in naloxone administration empowers individuals to take immediate action during overdose emergencies.
Naloxone Training for Laypeople
- Accessible Community Workshops: Naloxone training sessions are often conducted in community centers, schools, and other public venues to reach a broad audience.
- Overcoming Barriers to Participation: Efforts are made to eliminate barriers such as cost and time constraints to encourage widespread participation in naloxone training programs.
- Building a Naloxone-Ready Society: By equipping individuals with the knowledge and tools to respond to opioid overdoses, society becomes better prepared to save lives and reduce overdose-related fatalities.
Conclusion: Naloxone’s Crucial Role in Opioid Safety
Naloxone has emerged as an indispensable tool in the fight against opioid overdoses, offering a lifeline to those facing life-threatening situations. From its inception as an emergency intervention to its integration into various settings and populations, naloxone continues to make a profound impact on public health. Through innovative distribution strategies, increased awareness, and ongoing research, naloxone’s life-saving potential is poised to grow even further, making the world a safer place in the face of the opioid crisis.
Frequently Asked Questions (FAQs) about Naloxone and Opioids
1. What is the role of naloxone in opioid overdose reversal?
Naloxone is an opioid receptor antagonist that rapidly binds to opioid receptors, displacing opioids and reversing the effects of an overdose. It restores normal breathing and can be life-saving in opioid emergencies.
2. Can naloxone be used for non-opioid overdoses?
Naloxone is specifically designed to reverse opioid overdoses and may not be effective for other drug overdoses. It works by targeting opioid receptors, so it is not effective against non-opioid substances.
3. Is naloxone safe to use in pregnant individuals?
Naloxone is considered safe for use during pregnancy, as it does not have direct opioid effects and poses no risk of dependence. Administering naloxone in cases of opioid overdose is crucial to protecting both the pregnant individual and the fetus.
4. How long does naloxone’s effects last in the body?
The duration of naloxone’s effects varies based on factors such as the individual’s metabolism and the opioid’s half-life. Generally, naloxone’s effects last for about 30-90 minutes, and additional doses may be necessary if the opioid remains in the system.
5. Can naloxone be harmful if administered to someone without opioid overdose?
Naloxone only affects individuals who have opioids in their system and is not harmful if given to someone without opioid use. It is safe to administer naloxone as a precaution if opioid overdose is suspected.
6. How can I access naloxone for personal use?
Naloxone is available through various channels, including pharmacies, harm reduction organizations, and healthcare providers. In many regions, individuals can obtain naloxone without a prescription.
7. Does naloxone lead to withdrawal symptoms in individuals with opioid dependence?
Naloxone’s rapid reversal of opioids can precipitate withdrawal symptoms in individuals with opioid dependence. However, the primary goal is to save lives during an overdose, and the benefits of administering naloxone outweigh the temporary discomfort of withdrawal.
8. Are there any side effects of naloxone administration?
Naloxone is generally well-tolerated and safe. Side effects may include nausea, vomiting, headache, and restlessness. These side effects are temporary and resolve quickly.
9. Can bystanders administer naloxone without formal training?
Yes, bystanders can administer naloxone without formal training. Naloxone kits often come with simple and clear instructions for use, making it accessible for individuals without medical expertise.
10. Can naloxone be used for fentanyl and other synthetic opioids?
Yes, naloxone is effective in reversing overdoses caused by fentanyl and other synthetic opioids. It is essential to have naloxone readily available due to the increasing prevalence of potent synthetic opioids in the illicit drug market.
Related posts:
- How Long Does Naloxone Last? Exploring the Duration of Naloxone’s Effects14 min read
- How Long Does Naloxone Block Opiates? Find Out Now!18 min read
- Does Naloxone Block Benzos? Discover the Surprising Interactions.13 min read
- How Much Does Naloxone Cost Without Insurance: Affordable Solutions for Opioid Overdose14 min read